Two weeks ago we posted the Blog titled “Nursing Home Blues”. Terry contacted me after she read the article and we began exchanging emails. As we corresponded it become more and more evident to me that Terry’s experience is not unique. Many people are dealing with what Terry and her family are living through. As dementia symptoms increase throughout our country more lives than just the patient’s are affected. It is also evident that as a society we are not addressing the increasing need of providing appropriate care for these many individuals and their families.
With Terry’s permission I have included parts of our correspondence. It points to a need but unfortunately not a solution. My hope is other people reading this blog will share comments and ideas.
Dear Barbara, your blog, Nursing Home Blues, touched a nerve, so I reach out to you. This is an area that is in such need of review and transparency...having been exposed to almost every type of living arrangement for my mother, from Assisted Living, to locked Memory Care, living at home with caretakers, and then a series of what is termed 'health and rehab' facilities, I have found there is such a disparity between what is advertised, and what is real. And finding a 'nursing home' that consistently cares is impossible, I have decided. I used the spend down method of getting my mom into Medicaid coverage, but we were careful about visiting and asking questions all along the way. Even the best proved to be less than supportive toward dementia patients, and seemed to have a profile that all were expected to fit into, otherwise they were labelled 'combative' and proved difficult, if not impossible, to place. Someone who was not wheelchair or bed-bound, as my mother was not, was deemed to be 'too much trouble' because of the need for more contact and interaction.
I understand burn out, and having bad days, but kindness and caring are in low esteem by facilities, especially when watching the bottom line. Fortunately, I suppose, my mother is now bed-bound and we were able to get Hospice to help out, so she now fits the bill for a 'model patient'... but it still seems one nurse can wreck her entire day with a bad attitude at changing time or bath time. And family (which is me) must try to piece back together a mindset that keeps her contented and unafraid. This is a sad time of life. And I do have the Nursing Home Blues, quite regularly. Another good topic for someone like yourself, would be 'The Business of Dying' which I am hoping to delve into one day....people who are facing the prospect of a terminal illness need to know that it is a business, basically, and they should try to understand how to fit into the system. Just my thoughts.
Terry
Hi Terry, I appreciate your reply. You are so right about the challenges of finding appropriate care for many of our not so incapacitated citizens (because you are living it).
I agree with your ideas on "the business of dying". Treatment is paid for by insurance, Medicare, Medicaid. Treatment puts a lot of fancy cars in healthcare provider’s garages. I have very strong feelings about physicians and clinics charging for administering therapies and drugs. Physicians should not be benefiting financially from administering and/or the drugs they are prescribing. I see that as a conflict of interest and certainly deserves a second, or even third opinion.
When "treatment" fails or is not accepted there is a severe lack of services that are paid for by insurance, Medicare and or Medicaid. At a time when people need the most help there are few payment options outside of private pay. Hospice and palliative care does not pay for continuing room and board in any facility ,or for in home custodial care. Those two areas represent the most need for those with dementia, yet there is little if any financial help available.
I don’t have answers or even ideas for how to change this lack in our healthcare system. Let’s get a discussion started.
Blessings,
Barbara
Something more about Nursing Home Blues Part 2...
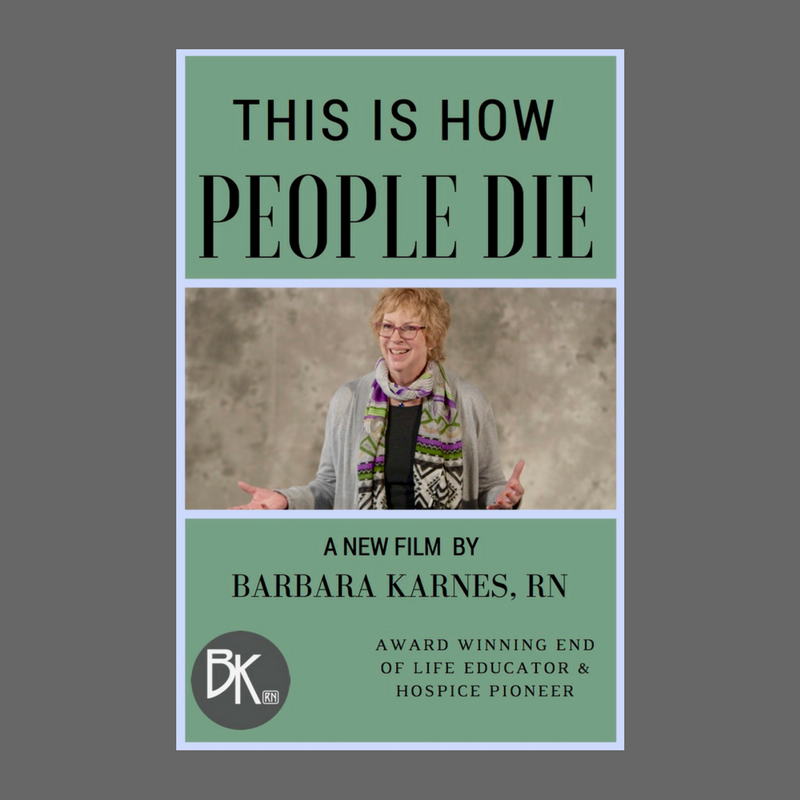
As I think about "the business of dying" I think about how helpful my short film NEW RULES for End of Life Care. After watching the film most viewers are struck by the fact that we don't need medical intervention to die. Dying is not a medical event. No one needs a doctor or a nurse or to be in the hospital when they're close to death. But the medical community encourages it. Watch the film and have your eyes opened and then share it with your family, your church, your community. Let's all be educators on the normal way people die.







8 comments
Susan Mason
Every patient in a Nursing Home must have an advocate for them. Unfortunately so many do not. As a Hospice Volunteer coordinator I have seen first hand what our hospice volunteers do for these folks that are at the end of their life. Our volunteers almost adopt the patient and come to see them as much as possible. If they see or hear something they do not like they will call me and I will contact the hospice nurse. All of our volunteers know the golden rule and I speak of it often. “Treat others just like you would want to be treated”! What if that was you laying in the bed….would you want to be ignored? A shout out to all volunteers that go to nursing homes and bless these special patients!!!
Every patient in a Nursing Home must have an advocate for them. Unfortunately so many do not. As a Hospice Volunteer coordinator I have seen first hand what our hospice volunteers do for these folks that are at the end of their life. Our volunteers almost adopt the patient and come to see them as much as possible. If they see or hear something they do not like they will call me and I will contact the hospice nurse. All of our volunteers know the golden rule and I speak of it often. “Treat others just like you would want to be treated”! What if that was you laying in the bed….would you want to be ignored? A shout out to all volunteers that go to nursing homes and bless these special patients!!!
Barbara Karnes
Hi Linda, in response to your email about your mother’s experience in a nursing facility, unfortunately your story is way too familiar. As we live longer and our population has increased nursing facilities are just not meeting the many needs that residents have. Shortage of staff and the high rate of staff turnover is a major component to this troubling situation.
What can we do? Report inappropriate or lack of care to regulating agencies when you see it. However I don’t think it is abuse that occurs in most cases it is just that we want more for our loved ones in institutions than the basics of care. We want our loved ones given the kind of personal care that due to whatever circumstances we ourselves can’t provide.
Again what can we do? We can follow your example—visit daily, interact with the personnel, bring favorite foods, if possible take your special person out for an adventure (even if it is just a drive). The sense of being isolated by and from family and friends is a huge component to a unhappy and unpleasant experience.
Linda, thank you for asking. As I reread this email I see that I really don’t have an answer for you. I agree there is a problem but I don’t know how to fix it (and that is very frustrating for this fix it personality.)
Hi Linda, in response to your email about your mother’s experience in a nursing facility, unfortunately your story is way too familiar. As we live longer and our population has increased nursing facilities are just not meeting the many needs that residents have. Shortage of staff and the high rate of staff turnover is a major component to this troubling situation.
What can we do? Report inappropriate or lack of care to regulating agencies when you see it. However I don’t think it is abuse that occurs in most cases it is just that we want more for our loved ones in institutions than the basics of care. We want our loved ones given the kind of personal care that due to whatever circumstances we ourselves can’t provide.
Again what can we do? We can follow your example—visit daily, interact with the personnel, bring favorite foods, if possible take your special person out for an adventure (even if it is just a drive). The sense of being isolated by and from family and friends is a huge component to a unhappy and unpleasant experience.
Linda, thank you for asking. As I reread this email I see that I really don’t have an answer for you. I agree there is a problem but I don’t know how to fix it (and that is very frustrating for this fix it personality.)
Linda Hopkins
Barbara – thanks for all your work. Your booklets and blogs have been very helpful to me.
My mom passed away last July in a new private, Assisted Living Memory Care facility in Northbrook, IL. It was nothing like some of the stories above, so I need to be very grateful for that. It was physically beautiful – and expensive – but it was understaffed, with a fair amount of turnover, a weak activities program and the caregivers assigned to work as the waiters / waitresses, meaning they didn’t have time to help the patients.As a result, there was really no personal interaction with the patients (saying “hi” and “do you have to go to the bathroom” do not count). I felt I needed to pay for additional care givers for my mom and visit nearly every day to be sure she was well cared for and had someone to talk to. Basically, the place provided decent personal care (toileting, bathing, etc.), average food but no one to facilitate at meals, not great activities and poor social support. I will say that their Dr. didn’t seem to push meds. It never came close to my naive expectations – but given others’ stories, it sounds like paradise — How sad.
We wound up there because i couldn’t get medical support from her doctor – i could never reach him and the nurses answer to everything was “take to to the emergency room” – a terrible experience every time, that always turned out to be a bladder infection. After the last hospital stay, her time in the rehab was terrible – i’m so sorry i accepted that.
Anyway – I wish there were much better alternatives.
How do you think we can help???
Barbara – thanks for all your work. Your booklets and blogs have been very helpful to me.
My mom passed away last July in a new private, Assisted Living Memory Care facility in Northbrook, IL. It was nothing like some of the stories above, so I need to be very grateful for that. It was physically beautiful – and expensive – but it was understaffed, with a fair amount of turnover, a weak activities program and the caregivers assigned to work as the waiters / waitresses, meaning they didn’t have time to help the patients.As a result, there was really no personal interaction with the patients (saying “hi” and “do you have to go to the bathroom” do not count). I felt I needed to pay for additional care givers for my mom and visit nearly every day to be sure she was well cared for and had someone to talk to. Basically, the place provided decent personal care (toileting, bathing, etc.), average food but no one to facilitate at meals, not great activities and poor social support. I will say that their Dr. didn’t seem to push meds. It never came close to my naive expectations – but given others’ stories, it sounds like paradise — How sad.
We wound up there because i couldn’t get medical support from her doctor – i could never reach him and the nurses answer to everything was “take to to the emergency room” – a terrible experience every time, that always turned out to be a bladder infection. After the last hospital stay, her time in the rehab was terrible – i’m so sorry i accepted that.
Anyway – I wish there were much better alternatives.
How do you think we can help???
Claudia Hauri
For knowledge about the dying process get Barbara’s book ‘The Final Act of Living’ I heard Barbara speak at Univ. of Miami years ago, & her experience helped my with my mom die at her condo, 24/7 care, with Hospice, just shy of her 101 birthday.
As a Nurse Practitioner ( 40 yrs) I regretfully say that there is few & far between residential care facilities at ANY level that are above a 4 ( (1=low, 10= tops).
Save, save, save, get Long Term Care if possible, contact a church for volunteer help, check with Office/Dept. of Affairs for resources, ask the health care provider for a prescription for care for possible income tax reduction/dependency of person.
Then care for yourself knowing you have done your best.
In Miami the cost of the last year was about $ 50-52,000/year.
For knowledge about the dying process get Barbara’s book ‘The Final Act of Living’ I heard Barbara speak at Univ. of Miami years ago, & her experience helped my with my mom die at her condo, 24/7 care, with Hospice, just shy of her 101 birthday.
As a Nurse Practitioner ( 40 yrs) I regretfully say that there is few & far between residential care facilities at ANY level that are above a 4 ( (1=low, 10= tops).
Save, save, save, get Long Term Care if possible, contact a church for volunteer help, check with Office/Dept. of Affairs for resources, ask the health care provider for a prescription for care for possible income tax reduction/dependency of person.
Then care for yourself knowing you have done your best.
In Miami the cost of the last year was about $ 50-52,000/year.
Terry Camper
Don, so many patients in the facility where my mother lives do not have anyone to ‘go to bat’ for them, and I have such sympathy for their situation. I do what I can to speak kindly, offer an assist when possible, or just smile and say hello. These simple gestures mean so much to some of them, but more often I am in a hurry to get back to my own mother, and with her now bed-bound, I see fewer of them, less often. Volunteer organizations are great, but I wholeheartedly agree that career counseling is a very real need in most of these nursing facilities, and often in hospitals, too. I’ve see such a range of ability and compassion in the ‘social worker’ field as well. I hope things are good for you and your wife at this point.
Don, so many patients in the facility where my mother lives do not have anyone to ‘go to bat’ for them, and I have such sympathy for their situation. I do what I can to speak kindly, offer an assist when possible, or just smile and say hello. These simple gestures mean so much to some of them, but more often I am in a hurry to get back to my own mother, and with her now bed-bound, I see fewer of them, less often. Volunteer organizations are great, but I wholeheartedly agree that career counseling is a very real need in most of these nursing facilities, and often in hospitals, too. I’ve see such a range of ability and compassion in the ‘social worker’ field as well. I hope things are good for you and your wife at this point.
Nancy Buckingham
Oh!! This does strike a nerve with me. I too am too familiar with many of thes me facilities. My mother was in one for 4 years and we had private sitters. For the past 21 months I have been taking care of my husband and the facilities are worse than what they used to be! Fortunately he’s at home on hospice and I know this has extended his life. He is bedridden, his mind is good some days and other times he is confused.. but most of the time he’s a great patient! I have my brother helping me as he lives with me, I have 2 daughters, one in Nashville that helps out every month!! And my other daughter lives here and has helped out tremendously. I was diagnosed with breast cancer last Oct., had surgery in Nov and radiation in January! Challenging times, however back to the facilities, they need a makeover!! These patients are being treated terribly. My husband is in this condition because an aide helped him go to the bathroom and did not help him get back to bed. It’s sickening what they allow. This facility did not have any liability insurance so therefore there is no legal direction that we can take! New laws need to be made!!
Oh!! This does strike a nerve with me. I too am too familiar with many of thes me facilities. My mother was in one for 4 years and we had private sitters. For the past 21 months I have been taking care of my husband and the facilities are worse than what they used to be! Fortunately he’s at home on hospice and I know this has extended his life. He is bedridden, his mind is good some days and other times he is confused.. but most of the time he’s a great patient! I have my brother helping me as he lives with me, I have 2 daughters, one in Nashville that helps out every month!! And my other daughter lives here and has helped out tremendously. I was diagnosed with breast cancer last Oct., had surgery in Nov and radiation in January! Challenging times, however back to the facilities, they need a makeover!! These patients are being treated terribly. My husband is in this condition because an aide helped him go to the bathroom and did not help him get back to bed. It’s sickening what they allow. This facility did not have any liability insurance so therefore there is no legal direction that we can take! New laws need to be made!!
Kathleen Clohessy
An interesting discussion and a much overlooked topic, particularly the reference to providers (e.g. doctors and hospitals) pushing aggressive, unnecessary, and futile care at the end of life. And though I agree that our for-profit healthcare system bears much of the blame for that, it is also true that the public MUST become more informed and aware about their choices at the end of life. And they must communicate to everyone within earshot what what they do and do not want long before they are being wheeled into the emergency room after a panicked family member calls 911 and “wants everything done.”
An interesting discussion and a much overlooked topic, particularly the reference to providers (e.g. doctors and hospitals) pushing aggressive, unnecessary, and futile care at the end of life. And though I agree that our for-profit healthcare system bears much of the blame for that, it is also true that the public MUST become more informed and aware about their choices at the end of life. And they must communicate to everyone within earshot what what they do and do not want long before they are being wheeled into the emergency room after a panicked family member calls 911 and “wants everything done.”
Don Eisenberg
Barbara, I agree about Terry’s comment that it only takes one out-of-sorts caregiver to shatter the patient’s day and peace, and require much more effort on the part of family and others to then “right the ship.” Some years ago my wife was in a cancer unit of a major hospital, after we’d learned her breast cancer had metastasized. While I was at work, the social worker (of all people) came in and told her “I’ve been fighting with the insurance people since you came here- you’re going to have to leave!” Needless to say, I had a “come to Jesus meeting” with a top administrator a few hours later to suggest some career counseling for the young social worker. They then transferred my wife to the “transitional unit” in the same facility in order to satisfy the insurance requirements. I can only imagine what happens to people who do not have someone to “go to bat” for them.
Barbara, I agree about Terry’s comment that it only takes one out-of-sorts caregiver to shatter the patient’s day and peace, and require much more effort on the part of family and others to then “right the ship.” Some years ago my wife was in a cancer unit of a major hospital, after we’d learned her breast cancer had metastasized. While I was at work, the social worker (of all people) came in and told her “I’ve been fighting with the insurance people since you came here- you’re going to have to leave!” Needless to say, I had a “come to Jesus meeting” with a top administrator a few hours later to suggest some career counseling for the young social worker. They then transferred my wife to the “transitional unit” in the same facility in order to satisfy the insurance requirements. I can only imagine what happens to people who do not have someone to “go to bat” for them.